Dry Eye Clinic
Dry Eye Disease, Blepharitis and Meibomian Gland Dysfunction
Dry eyes; what's the fuss?
Dry eyes can become a very painful and debilitating condition. DED (Dry Eye Disease) is more common than people may think and according to the DEWS 2 (Dry Eye Workshop Study 2) report in 2017, this condition affects hundreds of millions of people around the world. It is one of the main reasons why many patients visit their optometrist.
Do you suffer from pink, gritty, sore or tired eyes?
If the answer is yes, then you may be one of the millions of people who suffer from DED (dry eye disease). It is estimated that the condition affects 1 in 5 people. To understand your condition, at Goldwyn Opticians, your optometrist will ask you to complete a tear film questionnaire. This is also known as the Ocular Surface Disease Index 2 (OSDI 2). See here for a sample of OSDI 2:
Do you suffer from a watery eye?
Excessive watering can be caused by the dryness. To compensate, the eye produces more water to combat the dryness and this often leads to over tearing. This can be a problem for most people on a cold windy day, but those suffering from DED can experience watery eyes more often.
Why does it happen?
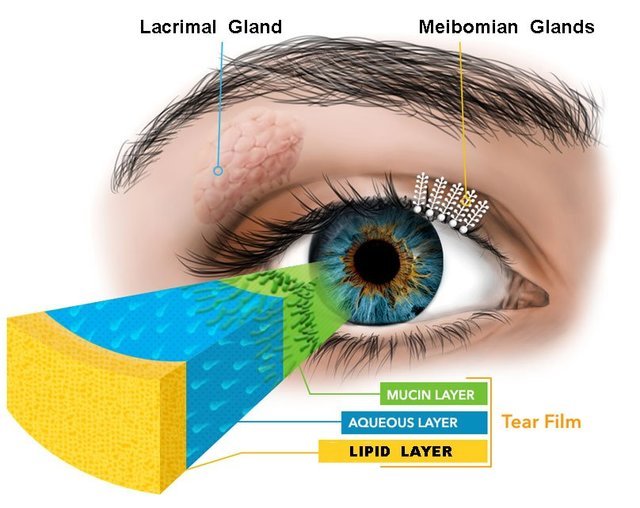
An unstable tear film. The tears your eyes produce may be deficient in quantity or quality, or they simply evaporate too quickly. A normal tear film is around 3 microns thick and is made of three distinct layers; (1) the mucin layer, a sticky layer that helps the tear film bind to the cornea. Mucin is made in the conjunctival goblet cells, (2) the aqueous layer or the watery later. This is the bulk of the tear film and carry the nutrients, defence agents and gives clear vision. Aqueous is made and secreted by the lacrimal gland (3) the lipid or oily layer, essentially stops the tears from evaporating. It is produced in the meibomian glands in the eyelids. See diagram:
What triggers dry eyes?
Other than ageing and poor health, prolonged use of computer/smart devices, exposure to air conditioning, central heating, pollution, side effects to medicine, smoking, hormonal changes, contact lenses wear and eye surgery are some of the risk factors. Studies have shown that more women suffer from DED compared to men. At Goldwyn Opticians, we will conduct a detailed history and symptoms exercise to investigate risk factors that may affect you.
What can be done?
The good news is that DED can be managed with several products including sodium hyaluronate based eye drops, tea tree oil lid wipes and moist heat masks.
Should I visit my GP?
If your GP is not trained in eyes and dry eyes management, the chances are that you may end up with preservative based Hypromellose or Sno-Tears eye drops. This is now old practice and we have far better unpreserved products to give dry eye relief.
Who can come to us?
You can simply call in and request a dry eye assessment. We can take referrals from GPs and other opticians whose patients have tried a number of treatments without success. We will devise an individual treatment plan for you including follow up visits to monitor your tear film.
What does it cost and involve?
Your appointment will last around 20 minutes with the optometrist and will cost £23. Dry eye assessment is not funded by the NHS. We will take a detailed history and symptoms including a tear film questionnaire, use fluorescein sodium to assess the tear film quality and ocular surface, assess the underside of the eyelids, assess the eyelid margin and the orifices of the meibomian glands, assess the tear ducts, assess your blink rate and response, assess your tear break-up time (TBUT), assess your tear meniscus and make recommendations for treatment/management.
What else can I do that will help?
To educate yourself is stage one. Understanding and coming to terms with dry eye disease will make treatment more effective and increase changes of relief. Investing in a humidifier at home or work can help. Drinking water will certainly help. An adult should drink around 2 litres of water/clear fluid daily. Omega 3 oils found in food like fish and food supplement will help with managing DED. Your GP may need to review your medication. We will always advise preservative free dry eye drops. Regular eyelid hygiene and warm compresses go a long way.
Using baby shampoo as traditional lid hygiene?
As members of the College of Optometrists, we do not recommend the use of Johnsons baby shampoo or any other shampoo to treat blepharitis. If you have been advised by a doctor to use this off-license, then this is something we cannot advise you on. There are specifically designed more convenient alternatives that have proven effectivity on blepharitis. Speak to our optometrists.